Introduction
Prostate cancer represents one of the main causes of malignancy in the world and the leading cause of cancer in men1. Epidemiologically, a figure of 1,467,000 cases/year was reported for 2023, representing 7.34% of the total number of cancer cases reported, ranking it as the fourth most frequent type of cancer, surpassed by mama, lung, and colorectal cancer2. At present, the estimated worldwide mortality rate for prostate cancer is 27.1%, with the central regions affected being the African continent in its southern, middle, and western zones, followed by Latin America and the Caribbean. Finally, in Polynesia, where estimated mortality rates reach 20%3, in Colombia, the estimated number of prostate cancer cases is 16,479 cases, with an estimated mortality rate of 7.6%, being the second most frequent type of cancer after breast cancer4.
Late diagnosis of prostate cancer currently represents one of the leading causes of mortality risk for this disease5. Late diagnosis of prostate cancer is characterized by the involvement of the entire prostate gland and the risk of metastasis, affecting mainly bone and nearby lymph nodes, increasing the risk of pathological fractures, disability, and early death6. Late diagnosis of prostate cancer increases the mortality, disability, and dependency rate by 48%, in addition to significantly increasing the cost of treatment and the aggressiveness of the disease7. The late diagnosis of prostate cancer increases the mortality rate, disability, and dependence in 48% of cases, in addition to significantly increasing the cost of treatment and the aggressiveness of this, especially leading to multimodal therapies that affect the quality of life of those affected8.
Several studies have shown that there are social and structural barriers or conditions that delay the early diagnosis of cancer, the most frequent being the rural origin of the patients, belonging to the female sex, belonging to an excluded ethnic/racial group, having a high workload and presenting episodes of previous depression that confuse the general malaise due to the oncological process with psychological causes, among others9,10. The main factors influencing late diagnosis of prostate cancer are socioeconomic and previous studies in Taiwan support that low-income men have a 44% higher risk of being diagnosed with late-stage prostate cancer than those who are considered high and middle-income, also increasing the risk of mortality in this population group from 3 to 111. Other studies developed in the U.S.A. have reported that African Americans are the leading population group that receives a late diagnosis of prostate cancer and in whom there is a higher risk of complications associated with the difficulty of accessing timely treatment12.
In low- and middle-income countries, such as Colombia, access to health care presents barriers and obstacles for specific population groups that have been marginalized due to cultural, historical, social, economic, political, and contextual issues, such as the armed conflict in the country13, these situations have led to prevention and screening strategies for early detection being inefficient in specific population groups and specific geographic areas and lead to thinking that there are country-specific sociodemographic conditions that directly influence the opportunities for treatment and prevention of prostate cancer complications. Different studies have shown that unequal access to health care in Latin America is one of the leading causes of prostate cancer mortality in the region. In countries such as Costa Rica, the lack of access to medical care has led to pockets of prostate cancer mortality in some areas despite similar clinical behavior of prostate cancer cases14.
Therefore, we aimed to estimate the relationship between certain sociodemographic variables, such as housing location, racial-ethnic linkage, and the diagnosis of advanced prostate cancer in patients with a clinical and histopathological diagnosis and residing in the departments of Valle, Cauca, and Tolima in Colombia.
Methods
Type of study
We conducted a retrospective observational study between 2020 and 2023 on patients with histological and clinical diagnoses of prostate cancer attending the Instituto Oncológico Ospedale S.A.S. sites and residents of the departments of Valle, Cauca, and Tolima.
Participants
INCLUSION CRITERIA
Patients with clinical and histopathological diagnoses of prostate cancer were included, with staging according to the T.N.M. criteria established by the European Society of Urology for the year 202315 and those attended by the Instituto Oncológico Ospedale S.A.S. sites in the Valle, Cauca, and Tolima departments from 2020-2023.
EXCLUSION CRITERIA
Patients with undefined staging according to T.N.M. criteria were excluded15, whether the information was unavailable or was yet to be defined at the time of diagnosis, the demographic variables necessary for the statistical analysis could not be completed, or those whose medical history could not be fully accessed due to insurance company issues. Patients only seen once by the institute were excluded since they were reassigned to other institutions due to insurance issues.
Variables
The variables were divided into three categories: First, the sociodemographic characteristics of the patients, including age, ethnic/racial affiliation, residence localization (if from a rural or urban area), the affiliation regime: contributory, private or subsidized, and the main primary caregiver (if any). Second, the clinical characterization, which included T.N.M. classification, initial prostate-specific antigen (P.S.A.), ISUP, and Gleason Scale, establishing and classifying the patient groups into two: metastatic (IV) and non-metastatic (I-III), the presence of comorbidities or clinical history of importance, signs, and symptoms described (mainly urological) during diagnosis, presence of metastasis, type of metastasis and anatomical structures affected at the time of diagnosis. To establish the patient’s status, the Evaluation Criteria in Solid Tumors 1.1 (RESCIT 1.1) scale was used, establishing five primary outcomes: Complete Resolution, Partial Resolution, Stable Disease, Disease Progression, and Deceased, using imaging elements and biochemical markers such as P.S.A. to establish the status16.
Finally, the treatment modalities, where four main variables were included: surgical treatment, including prostatectomy and orchiectomy, radiotherapy, chemotherapy, and hormonal therapy, establishing which regimens or modalities were received, whether single or multiple. Evaluating also the opportunities for treatment and continued care, the date of issue of the pathology was considered as diagnostic confirmation and the first effective appointment with specialists in Urology, Uro-oncology, and/or Oncology.
Statistical analysis
UNIVARIATE DESCRIPTIVE ANALYSIS
For numerical variables such as age, treatment opportunities, and P.S.A. (i), among others, we averaged the data obtained and determined the standard deviation, establishing confidence intervals. For qualitative variables, we estimated the frequency of occurrence distinguished by the department.
BIVARIATE ANALYSIS
For this analysis, the population was divided into two subgroups, one metastatic (IV) and one non-metastatic (I-III), comparing their demographic variables. Hypotheses of association between independent variables, such as sociodemographic and clinical variables, and the result variable (clinical stage of prostate cancer) will be evaluated using specific tests according to the type of variable, such as χ2 or Fisher’s test for categorical variables or t-test or Wilcoxon for continuous variables, according to the assumptions of the tests.
REGRESSION MODEL
With the bivariate analysis, a logistic regression model was established to establish the risk relationship between the sociodemographic variables and the late diagnosis of prostate cancer by calculating the odds ratios (OR) and its corresponding 95% confidence interval.
Ethics committee approval
This study was approved by the ehics and research committee of the Instituto Oncológico Ospedale S.A.S. on October 30, 2023, under code 002-2023.
Results
Sociodemographic characteristics
A total of 475 patients were included. Most were distributed in Valle del Cauca, with 308 (64.8%), followed by Cauca, with 106 (22.3%), and lastly, Tolima, with only 61 (12.8%). An average age of 73.0 (8.68) for the diagnosis of prostate cancer, the department of Valle the one with the highest average age of 74.5 (8.57) for the diagnosis of prostate cancer. In terms of ethnicity/race, only 10.6% of the population was Afro-descendant, and the majority recognized themselves as mestizo. Regarding affiliation to the health system, the majority belonged to a subsidized scheme, 261 (54.9%), followed by the contributory scheme, 208 (43.8%), and finally, individuals or independent payers only 6 (1.3%). All patients are affiliated with a health insurance company and have an average treatment opportunity of 10.6 days after diagnostic confirmation, considering the issuance of the pathology until the first appointment with the specialist as a starting point (Table 1).
Table 1. Socio-demographic characteristics
| Department | Residence location | Ethnic/Race | Affiliation regime | Age | Primary caregiver* | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | Afro descendent | Mestizo | Subsidy | Contributive / particular | Mean (SD) | Women | Men | No report | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Valle | 197 (64) | 111 (36) | 31 (10.1) | 277 (89.9) | 120 (39) | 188 (61) | 74.5 (8.57) | 243 (79) | 16 (5.2) | 49 (15.2) |
| Cauca | 52 (49) | 54 (51) | 5 (4.7) | 101 (95.3) | 97 (91.5) | 9 (8.5) | 73.3 (8.43) | 92 (86.6) | 5 (4.7) | 9 (8.5) |
| Tolima | 24 (39.4) | 37 (60.6) | 0 (0) | 61 (100) | 44 (72.1) | 17 (27.9) | 69.8 (9.11) | 46 (75.4) | 5 (8.2) | 10 (16.4) |
|
* Person in charge of the care and attention of the oncology patient. |
||||||||||
Most of the support network or primary caregivers are women, of whom 331 (69.7%) corresponded to the patients’ daughters, partners, or wives. Only 24 (5.1%) were sons fulfilling this role, 64 (13.5%) were also women but nieces and sisters of the patients, and 15 (3.2%) corresponded to external caregivers.
Clinical and histological characterization
According to T.M.N. criteria, the non-metastatic population was 292 (61.5%), and the metastatic population was 183 (38.5%). Within the non-metastatic population, the majority was classified as stage II 131 (44.9%) (Fig. 1).
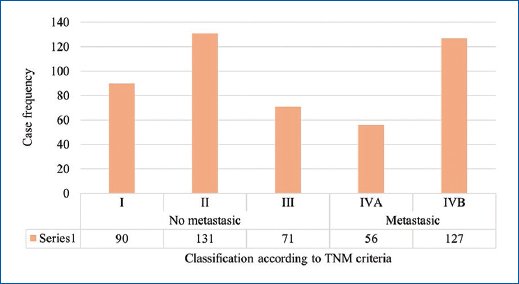
Figure 1. Classification of patients under study.
Among the most frequent urological signs and symptoms, hematuria was found to be the most frequent with 48 reports (10.1%), followed by pelvic pain with 46 (9.7%), and decreased urinary stream flow with 30 (6.3%) in third place. In the metastatic population, the main metastasis present was bone metastasis with 129 (70.5%), followed by lymph node metastasis with 81 (44.3%) and lung metastasis with 14 (7.7%) (Table 2).
Table 2. Clinical characterization
| Department | PSA (I) (ng/mL) | Initial urological signs and symptoms | Pathological fractures | Metastatic patients | Type of metastasis | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pelvic pain | Hematuria | Hematoespermia | Decrease in urine stream flow | Dysuria | Edema of the lower limbs | Erectile dysfunction | Bone/osteoblastic | Ganglionar | Pulmonary | Hepatic | Others* | ||||
| Mean (SD) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Valle | 74.9 (232.9) | 29 (9.4) | 29 (9.4) | 3 (1) | 21 (6.8) | 9 (2.9) | 3 (1) | 13 (4.2) | 2 (0.6) | 126 (41) | 92 (29.9) | 61 (19.8) | 12 (3.9) | 8 (2.6) | 2 (0.6) |
| Cauca | 92.3 (229.3) | 6 (5.7) | 15 (14.2) | 2 (1.9) | 5 (4.7) | 8 (7.5) | 3 (2.8) | 12 (11.3) | 1 (0.9) | 30 (28.3) | 16 (15.1) | 13 (12.3) | 2 (1.9) | 2 (1.9) | 1 (0.9) |
| Tolima | 77.5 (207.7) | 11 (18) | 4 (6.6) | 0 (0.0) | 4 (6.6) | 3 (4.9) | 1 (1.6) | 0 (0.0) | 1 (1.6) | 27 (44.3) | 21 (34.4) | 7 (11.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
|
PSA (I): initial prostate-specific antigen. * Others include brain and bladder metastasis. |
|||||||||||||||
Non-communicable chronic diseases were the main comorbidities identified in the population studied, the most frequent being hypertension, with 211 (44.4%), followed by diabetes mellitus type 2, with 92 (19.4%), and lastly, hypothyroidism, with 58 (12.2%) (Table 3).
Table 3. Medical history and co-morbidities
| Department | n (%) | ||||||
|---|---|---|---|---|---|---|---|
| Hypertension | Type 2 diabetes mellitus | Dyslipidemias | Chronic kidney disease | Other primary cancers | Hypothyroidism | Other pathologies | |
| Valle | 149 (48.4) | 70 (22.7) | 12 (3.9) | 7 (2.3) | 24 (7.8) | 45 (14.6) | 65 (21.1) |
| Cauca | 37 (34.9) | 17 (16) | 5 (4.7) | 0 (0) | 2 (1.9) | 1 (0.9) | 12 (11.3) |
| Tolima | 25 (41) | 5 (8.2) | 1 (1.6) | 0 (0) | 0 (0) | 12 (19.7) | 8 (13.1) |
The central systems affected by metastasis were the skeletal system and lymph nodes. Among the anatomical structures affected, we have mainly the pelvis with 80 (43.7%), followed by vertebrae with 77 (42.1%), and finally, the involvement of the axial skeleton with 70 (38.3%) of the reported cases. Regarding the lymph nodes affected, the inguinal lymph nodes were the most affected, with 49 (26.8%), followed by the thoracic with 19 (10.4%), and finally, the iliac with 11 (6%) of the reported cases (Table 4).
Table 4. Main anatomical structures affected by metastasis
| Department | n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Bone structures | Lymph nodes | |||||||||
| Pelvis | Axial skeleton | Vertebra | Ribs | Femur | Articulations | Inguinals | Iliacos | Obturator | Thoracic | |
| Valle | 56 (44.4) | 55 (43.7) | 59 (46.8) | 30 (23.8) | 18 (14.3) | 7 (5.6) | 38 (69.1) | 2 (3.6) | 1 (1.8) | 18 (32.7) |
| Cauca | 10 (33.3) | 6 (20) | 10 (33.3) | 5 (16.7) | 3 (10) | 0 (0.0) | 5 (35.7) | 9 (64.3) | 1 (7.1) | 1 (7.1) |
| Tolima | 14 (51.9) | 9 (33.3) | 8 (29.6) | 3 (11.1) | 2 (7.4) | 0 (0.0) | 6 (100) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Influence of sociodemographic factors on the diagnosis and follow-up of prostate cancer
The result of the bivariate analysis established that housing location, affiliation status, and age are sociodemographic factors that directly influence the chances of early diagnosis of prostate cancer (p < 0.05). Rurality seems to be one of the most influential factors in the late diagnosis of prostate cancer since, within the studied population, the majority of the metastatic population reported a rural origin (90.2%). They were followed by age, where persons classified as metastatic have a higher mean age of 74.2 (8.73) than non-metastatic 72.3 (8.58) at the time of diagnosis of prostate cancer.
As for the affiliation regime, statistically significant differences were also found between those affiliated to a state-subsidized regime (lower income capacity) and the contributory ones, finding that the subsidized ones have a higher risk of late diagnosis (metastatic). As for the support network, a distinction was made by gender, seeing that there were no statistically significant differences as a factor influencing late diagnosis of prostate cancer (Table 5).
Table 5. Bivariate analysis of the relationship between sociodemographic variables and patient groups and regression model
| Sociodemographic variable | Metastasic | No metastasic | Total | p* | OR | CI 95% lower | CI 95% upper |
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||||
| Residence location | 0.001 | 4.59 | 1.46 | 6.59 | |||
| Rural | 165 (90.2%) | 37 (12.7%) | 202 (42.5%) | ||||
| Urbana | 18 (9.8%) | 255 (87.3%) | 273 (57.5%) | ||||
| Affiliation regimen | 0.001 | 1.01 | 0.5 | 2.3 | |||
| Contributory or individual | 63 (34.4%) | 151 (51.7%) | 214 (45.1%) | ||||
| Subisidiated | 120 (65.6%) | 141 (48.3%) | 261 (54.9%) | ||||
| Age | 0.031 | 7.2 | 5.9 | 9.74 | |||
| Mean (SD) | 74.2 (8.73) | 72.3 (8.58) | 73.0 (8.68) | ||||
| Median (Min, Max) | 74.0 (53.1, 94.8) | 72.5 (49.4, 92.0) | 73.2 (49.4, 94.8) | ||||
| Primary caregiver (gender) | 0.092 | – | – | – | |||
| Female | 133 (72.7%) | 205 (70.2%) | 338 (71.2%) | ||||
| Male | 15 (8.2%) | 13 (4.5%) | 28 (5.9%) | ||||
| No report | 21 (11.5%) | 47 (16.1%) | 68 (14.3%) | ||||
| Parnert | 11 (6.0%) | 9 (3.1%) | 20 (4.2%) | ||||
|
* The p value is taken as p for statistically significant differences < 0.05. |
|||||||
Coming from a rural area is a risk factor for prostate cancer late diagnosis (OR = 4.59, 95% CI = 1.46-6.59) (Table 5). As for age, an OR = 1.01 (95% CI = 0.5-2.3). Furthermore, for the insurance an OR = 7.2 (95% CI = 5.9-9.74).
Modalities of treatment and monitoring
Regarding the status of the patients, it was found that most of the population studied had complete resolution of the disease 183 (38.5 %), followed by disease progression with 135 (28.4 %) and finally stable disease with 94 (19.8 %) (Fig. 2). As for the treatment modalities, these were grouped, finding that the treatment with the highest frequency of implementation was the hormonal treatment of androgen deprivation with 45.5% of cases, followed by active surveillance with 40.4%, and in third place, the combination of chemotherapy with hormone therapy (Fig. 3).
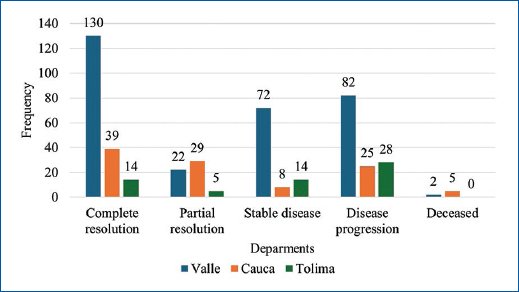
Figure 2. Present status of patients RECIST criteria 1.1.
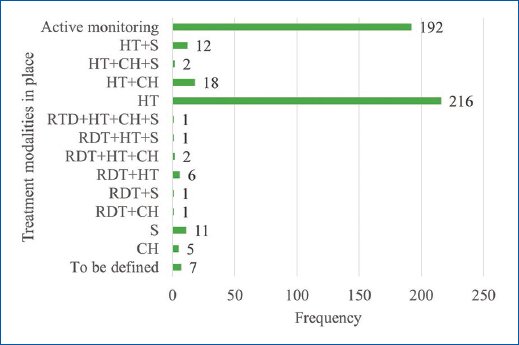
Figure 3. Treatment modalities in place. CH: chemotherapy; S: surgical; H.T.: hormonal therapy; RTD: radiotherapy.
Discussion
For the results obtained, this study presents results like those reported in the literature, where rurality is one of the main factors that influence the late diagnosis of prostate cancer17. Rurality has also been associated with lower treatment opportunities, higher risk of mortality, and lower possibility of adherence, becoming one of the critical factors influencing patient treatment and recovery18. Rurality has been associated with poverty and care difficulties. In the United States, it has been shown that there are differences even between black men from urban and rural locations, with a higher mortality rate in the latter and a higher risk of complications19. In other countries, such as Australia, rurality also represents an essential factor that influences not only the diagnosis but also the treatment and increases the risk of relapse by having less opportunity to access follow-up care20.
Racial status is also one of the factors influencing treatment opportunities, diagnosis, and adherence. In the United States, African American and Hispanic patients are more likely to have a late diagnosis of cancer, fewer opportunities for treatment, and more significant difficulties in accessing it, increasing their mortality rate compared to white men19. Although Latin America has a sizeable Afro-descendant population located mainly in the Caribbean, Brazil, and Colombia, there are so far no studies that evaluate the influence of social factors in the processes of diagnosis and management; only genetic elements have been determined as a risk factor for the development of prostate cancer21. As for the results obtained, it was not possible to evaluate the effect of racial ethnicity on the late diagnosis of prostate cancer since the Afro-descendant population included is very low, even though it represents 10% of the Colombian population and genetically has a higher risk of developing prostatic alterations22.
Concerning comorbidities, different studies have shown that metabolic alterations are the most prevalent in patients with prostate cancer, the main ones being hypertension, diabetes, and dyslipidemias, which were by the results obtained in our study23. However, it is essential to highlight that the comorbidity found was the presence of hypothyroidism; it is known that this condition by endocrine dysregulation increases the risk of cancer development, especially in young populations (< 60 years), being frequent in patients with lung and colon-rectal cancer, our study is the first that manages to demonstrate such a high prevalence of this condition in population with prostate cancer24,25.
Strengths and limitations
Among the strengths, this is the first study developed in Colombia that evaluates sociodemographic conditions and their association with the diagnosis of advanced prostate cancer, using three departments simultaneously located in southwestern Colombia, allowing us to reach accurate conclusions about the conditions and social determinants that influence the early diagnosis of prostate cancer and therefore, prevent the complications associated with it and reduce mortality rates in patients with late diagnosis.
One area for improvement in our study is that we did not perform an analysis that sought to see if there were inequalities within the urban population, which was the majority within our study population. The information in the medical records needed to be more sufficient to subclassify the participants by socioeconomic strata or level of education, since most medical records lacked this information.
Conclusions
Demographic conditions influence the chances of late diagnosis of prostate cancer in Colombia, with the main limiting factor increasing the risk of receiving more invasive therapies and reducing the probability of survival. Rurality is one of the main factors influencing the late diagnosis of prostate cancer in Colombia, as well as the affiliation regime, with the subsidy an influencing factor, and age, the older the age of diagnosis, the higher the risk of late diagnosis.
Funding
The authors declare that this work was carried out with the authors’ own resources.
Conflicts of interest
The authors declare that they have no conflicts of interest
Ethical disclosures
Protection of humans and animals. The authors declare that no experiments on humans or animals were performed for this research.
Confidentiality of data. The authors declare that they have followed their center’s protocols on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
